In any medical setting, patient safety and staff well-being are paramount. While we all strive for perfection, the reality is that incidents, big or small, can unfortunately occur. These might range from a slip and fall in the waiting room to a medication error or a data breach, and recognizing their potential impact is the first step towards a safer environment.
When an unexpected event happens, it’s not just about addressing the immediate issue; it’s about understanding what went wrong, why it happened, and how to prevent it from recurring. This crucial process of learning and improvement relies heavily on accurate and timely documentation. Without a clear record, valuable lessons can be lost, and risks might persist.
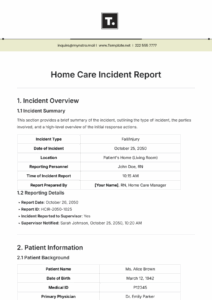
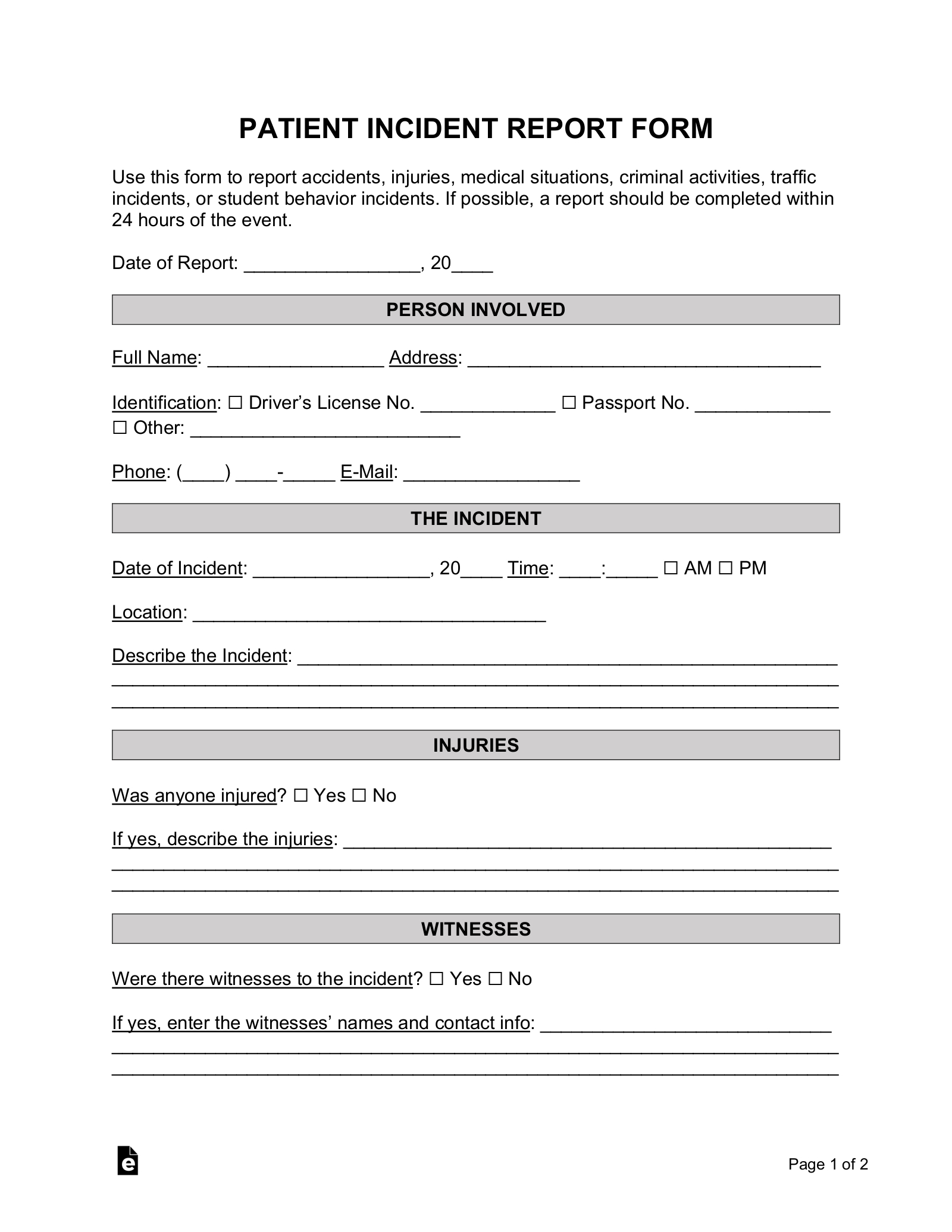
That’s where a well-designed incident report system becomes indispensable. Having a standardized approach ensures that every incident is captured consistently, providing the data needed to identify patterns, improve protocols, and ultimately enhance the quality of care and safety within your practice.
Why a Standardized Incident Report Template is Essential for Your Medical Practice
Adopting a standardized medical office incident report template is not just about fulfilling a bureaucratic requirement; it’s a foundational element of effective risk management and quality improvement. A consistent template ensures that every single incident, regardless of its perceived severity, is documented with the same level of detail and information. This uniformity prevents crucial details from being overlooked, providing a comprehensive picture for analysis. Without a consistent format, vital pieces of information might be missed, making it harder to piece together what truly occurred and what steps need to be taken.
Beyond mere documentation, a robust reporting system offers a layer of legal protection. Should an incident lead to a complaint or legal action, a meticulously completed incident report provides an objective, contemporary record of the event. This detailed account, including immediate actions taken and witness statements, can be invaluable in demonstrating due diligence and a commitment to patient safety, potentially mitigating liabilities and providing clarity in complex situations.
Furthermore, incident reports serve as powerful training tools. Each documented event offers an opportunity to review current procedures, identify gaps in staff training, or highlight areas where existing protocols might be insufficient or misunderstood. Analyzing these reports can reveal common human errors, equipment malfunctions, or environmental hazards, allowing your practice to implement targeted educational programs or update operational guidelines to improve overall performance and reduce future occurrences.
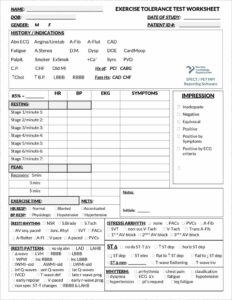
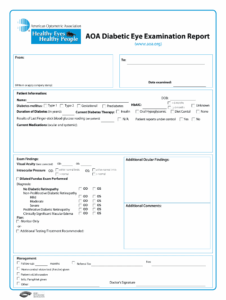
Key Elements Your Template Should Include
Finally, the cumulative data gathered from incident reports over time is gold. It allows your practice to identify trends, pinpoint recurring issues, and measure the effectiveness of corrective actions. This analytical capability is vital for proactive risk assessment, enabling you to move from a reactive response to incidents to a preventative strategy that significantly enhances the safety and efficiency of your medical office.
Implementing and Utilizing Your Medical Office Incident Report Template Effectively
Once you have chosen or developed a comprehensive medical office incident report template, the next critical step is ensuring its effective implementation across your entire practice. This isn’t a “set it and forget it” task; it requires clear communication, accessible resources, and consistent training for all staff members. Every employee, from front desk staff to clinical professionals, should understand what constitutes a reportable incident, where to access the template, and how to accurately complete it in a timely manner. Making the template easily available, perhaps through an accessible digital portal or a designated binder, removes barriers to reporting.
Beyond simply filling out the form, the real value of an incident report comes from the follow-up process. Reports should not just be filed away; they need to be reviewed promptly by a designated individual or committee. This review should involve an investigation into the root cause of the incident, an assessment of its impact, and a determination of necessary corrective actions. This might involve process changes, additional training, equipment maintenance, or even disciplinary measures, all aimed at preventing similar incidents in the future.
To truly maximize the benefits of your incident reporting system, consider these best practices for implementation:
Having a structured system for incident reporting is more than just a procedural task; it’s a proactive commitment to maintaining the highest standards of safety and care. By consistently documenting, analyzing, and acting upon incidents, your medical practice fosters an environment of continuous learning and improvement.
Embracing this methodical approach helps protect your patients, your staff, and your practice’s reputation. It reinforces a culture where safety is not just an aspiration but a tangible, achievable outcome, constantly refined through careful observation and responsive action.