In the complex worlds of clinical research and medical practice, the concept of informed consent stands as a foundational pillar. It’s more than just a signature on a form; it represents a profound ethical commitment to ensuring individuals fully understand and voluntarily agree to participate in treatments, procedures, or studies. This commitment safeguards patient autonomy and builds trust between healthcare providers, researchers, and the people they serve.
However, simply obtaining consent isn’t enough. The process of informed consent must be meticulously documented to stand up to scrutiny, whether for regulatory compliance, ethical review, or legal protection. This is where the challenges often arise. Without a standardized approach, essential details can be overlooked, leading to inconsistencies and potential complications down the line.
This article delves into the critical need for a structured framework to capture these vital interactions, exploring how a well-designed informed consent case report template can streamline documentation, enhance clarity, and reinforce ethical best practices in any setting where patient or participant consent is paramount.Why a Standardized Informed Consent Case Report Template is Crucial
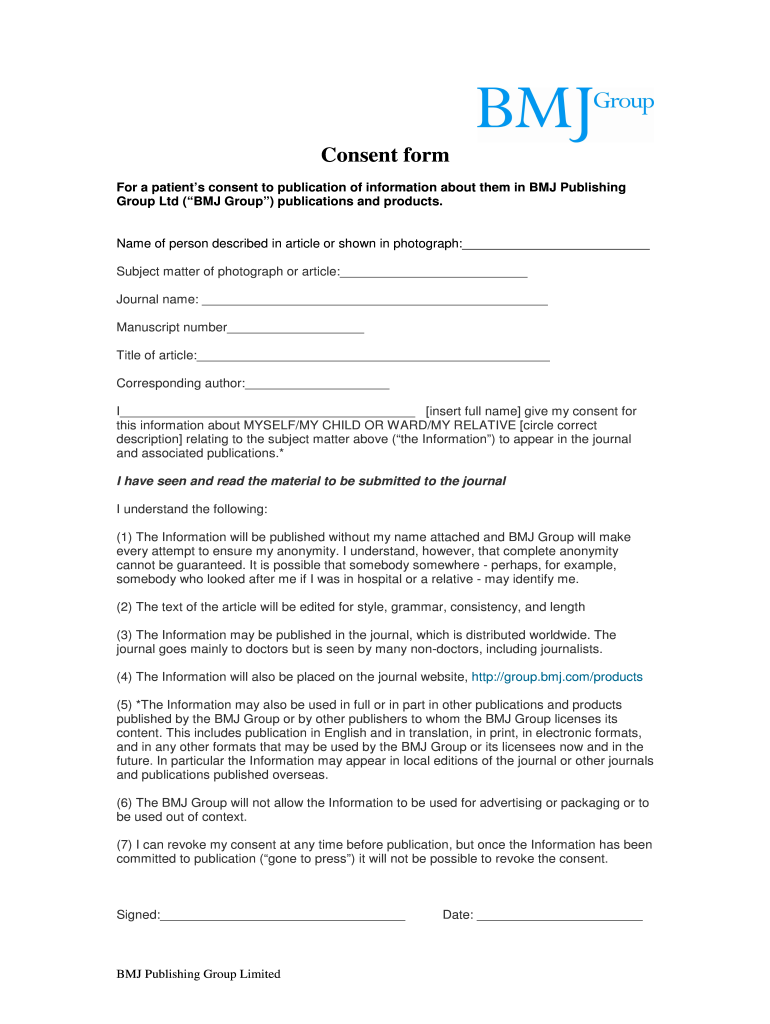
Navigating the ethical and legal landscape of medical procedures and research studies requires more than good intentions; it demands rigorous, consistent documentation. The informed consent process is often multifaceted, involving detailed discussions about risks, benefits, alternatives, and the participant’s right to withdraw. Without a clear, standardized method for recording these interactions, valuable information can be lost, potentially compromising patient safety, research integrity, and institutional accountability.
A standardized informed consent case report template serves as an indispensable tool, offering numerous benefits. It ensures consistency across all cases, regardless of who is conducting the consent discussion or documenting it. This consistency is vital for maintaining high ethical standards, facilitating internal reviews, and demonstrating compliance with regulatory bodies like the FDA or institutional review boards (IRBs). Moreover, a robust template provides legal protection by offering concrete evidence that a thorough and proper consent process was followed.
Think of the template as a comprehensive checklist that guides you through every critical step of the consent process, ensuring no stone is left unturned. It moves beyond merely confirming a signature, prompting the documentation of the dialogue that led to that signature. This structured approach helps in identifying any gaps in understanding or potential coercion, thereby strengthening the validity of the consent obtained.
Key Elements to Include in Your Template
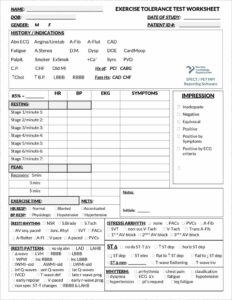
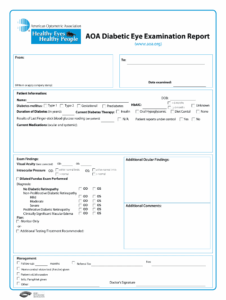
- Patient/Participant Demographics: Basic identifying information, often anonymized or coded for privacy, but sufficient for case tracking.
- Research/Treatment Protocol Details: A clear reference to the specific study or procedure for which consent is being sought, including protocol version numbers.
- Consent Process Documentation: Details on who conducted the consent discussion, the date and time, the language used, and any witnesses present.
- Information Provided: A list of the specific consent forms, patient information leaflets, or other documents provided to the individual.
- Risks and Benefits Discussion: Confirmation that all known risks, potential benefits, and alternative options were explained and understood.
- Voluntary Participation and Right to Withdraw: Documentation that the individual understood their participation was voluntary and they could withdraw at any time without penalty.
- Questions Answered: A note confirming that all questions asked by the individual were answered to their satisfaction.
- Signature and Date: Signatures of the participant/patient (or their legally authorized representative), the person obtaining consent, and any independent witnesses, along with the date.
The “Consent Process Documentation” element, in particular, goes beyond simply stating that consent was obtained. It captures the essence of the interaction, including the environment in which the discussion took place and any specific circumstances that might influence the participant’s comprehension or decision-making. This level of detail is invaluable when reviewing cases or addressing any future queries about the consent process.
Ultimately, neglecting to use a standardized informed consent case report template can lead to significant vulnerabilities. It risks accusations of ethical lapses, regulatory non-compliance, and even legal challenges, which can severely damage an institution’s reputation and impact its ability to conduct future research or provide care effectively. A meticulously completed template not only protects the institution but, more importantly, upholds the rights and dignity of every individual involved.
Practical Tips for Utilizing Your Informed Consent Case Report Template Effectively
Having a robust informed consent case report template is only the first step; its true value comes from its effective and consistent application. It’s not just about filling in blanks; it’s about fostering a culture of thoroughness and transparency. To maximize the utility of your template, ensure that all personnel involved in the consent process receive comprehensive training on its use. This training should cover not only what information to document but also the importance of each section and how to accurately reflect the nuanced conversations that take place during the consent discussion. Regular refresher sessions can help maintain high standards and address any evolving requirements.
Furthermore, consider the template as a living document, particularly in longitudinal studies or long-term treatment plans. Circumstances can change, new information might emerge, or a participant’s condition may evolve, necessitating re-consent or amendments to the original consent. Your template should ideally have sections to document these updates, including the dates of any re-consent discussions, the reasons for them, and any new information provided. This ensures a continuous and accurate record of the participant’s informed agreement throughout their involvement.
Finally, integrating the template seamlessly into your existing workflow is crucial. Whether you opt for a digital or paper-based system, ensure it’s easily accessible and user-friendly. For digital templates, consider features like automated date stamping, drop-down menus for common responses, and secure storage solutions that comply with data privacy regulations. For paper templates, ensure they are stored securely, are easily retrievable, and that there’s a clear process for archiving completed reports. The easier it is for staff to use, the more consistently and accurately it will be completed, strengthening your overall ethical and regulatory posture.
Meticulous documentation forms the bedrock of ethical practice and responsible research. By consistently utilizing a well-designed framework, institutions can ensure that every individual’s rights are respected and that all regulatory obligations are met with precision and clarity. It fosters an environment where trust is paramount and decision-making is truly informed.
Embracing a systematic approach to recording consent discussions not only mitigates risks but also elevates the quality of care and research. It empowers professionals to stand confidently behind their processes, knowing that every detail has been thoughtfully considered and properly preserved, contributing to a more transparent and accountable healthcare and scientific landscape for everyone involved.