Stepping into a new shift as a nurse often feels like walking into a complex puzzle. You’re taking over the care of patients you haven’t seen, relying entirely on the information passed on from your colleague. This critical exchange, known as the hand off report, is the bedrock of continuous, safe, and effective patient care. It’s where vital details about a patient’s condition, history, current status, and plan of care are meticulously transferred from one caregiver to the next, ensuring nothing falls through the cracks.
However, without a structured approach, these hand off reports can sometimes become inconsistent, hurried, or even miss crucial pieces of information. Imagine trying to remember every single detail about five or six patients, including their medications, pending lab results, family concerns, and the subtle changes in their condition, all while racing against the clock. It’s a challenge that can easily lead to misunderstandings, duplicated efforts, or, in the worst-case scenario, patient safety issues.
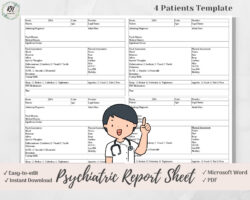
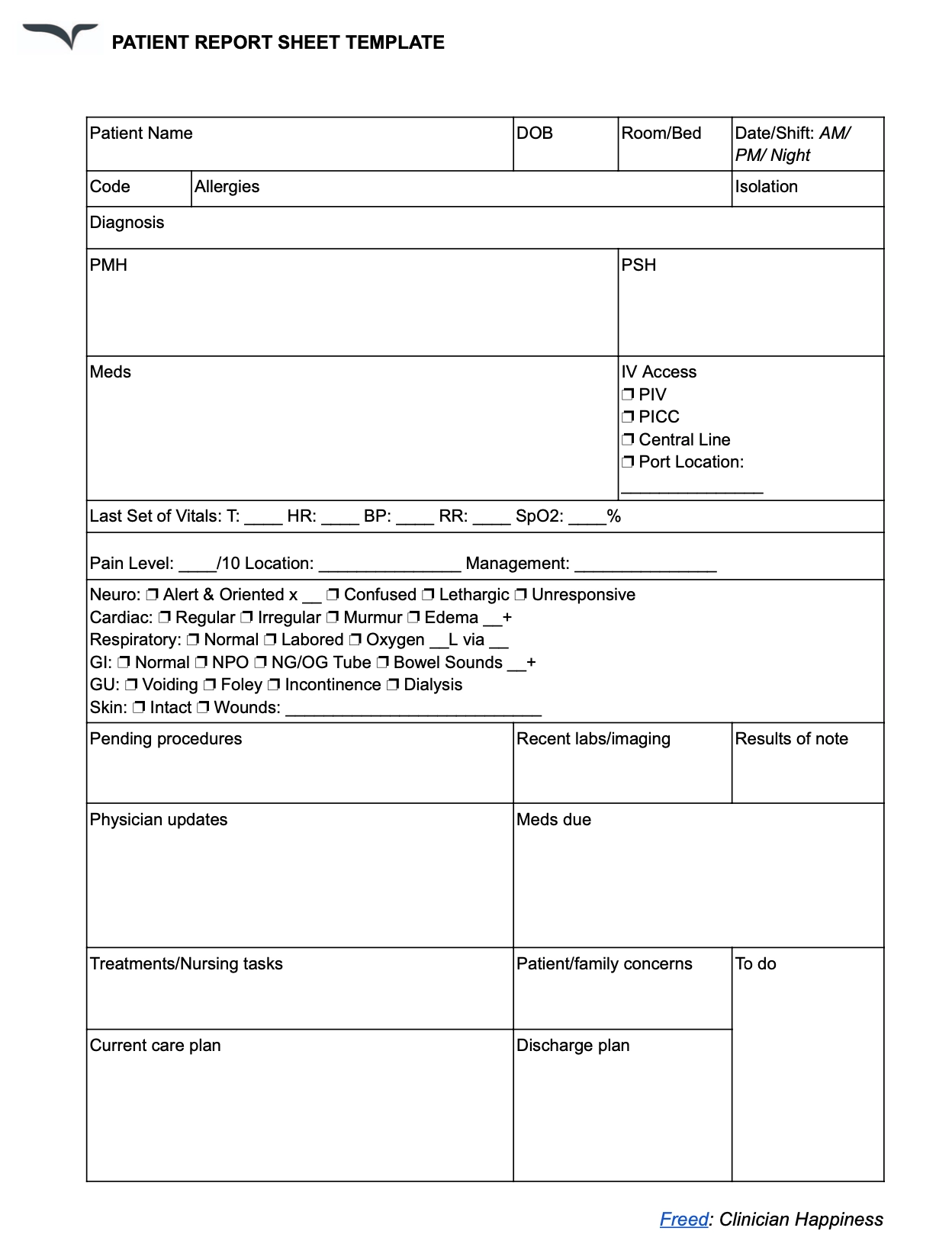
This is precisely where the power of a standardized nurse hand off report template comes into play. It provides a clear, consistent framework that guides nurses through the information exchange, ensuring all essential data is communicated thoroughly and efficiently. It’s not just about ticking boxes; it’s about creating a streamlined process that supports comprehensive patient care and fosters a safer environment for everyone involved.
Why a Standardized Nurse Hand Off Report Template is a Game-Changer
The difference a well-designed nurse hand off report template makes in a busy clinical environment is profound. Think about the common frustrations: nurses spending extra time hunting for information that wasn’t clearly passed on, or feeling anxious because they’re unsure if they have the complete picture. A template eliminates much of this guesswork and inefficiency, transforming a potentially chaotic process into an organized, reliable one. It ensures that every nurse, regardless of their experience level, follows the same logical flow for reporting, drastically reducing the chances of missed information.
Beyond just organization, a standardized template significantly boosts patient safety. When all critical data points are consistently addressed, from vital signs and assessment findings to pending orders and psychosocial factors, the risk of medication errors, delayed interventions, or overlooked changes in a patient’s condition decreases dramatically. It acts as a safety net, prompting nurses to consider all aspects of a patient’s care, fostering a culture of thoroughness and accountability.
Moreover, utilizing a specific nurse hand off report template can improve team communication and morale. When everyone is speaking the same language and following the same structure, communication becomes clearer and more concise. This efficiency frees up valuable time, allowing nurses to transition into their shift more smoothly and focus on direct patient care rather than deciphering incomplete reports. It also builds confidence among nurses, knowing they are both giving and receiving comprehensive, high-quality information.
From a legal and compliance perspective, a standardized template can also be invaluable. Detailed and consistent documentation during hand off reports provides a clear record of the patient’s status and the care plan at specific points in time. This robust documentation can be crucial in demonstrating adherence to care standards and institutional policies, offering an additional layer of protection for both the individual nurse and the healthcare facility. It truly elevates the standard of care across the board.
Key Elements Your Nurse Hand Off Report Template Should Include
A truly effective template isn’t just about listing things; it’s about capturing the essence of a patient’s story and their current needs. Here are some fundamental components that should be integrated into any robust nurse hand off report template to ensure a holistic and practical exchange:
- Patient Demographics and Identifier: Name, age, room number, and any relevant isolation precautions.
- Primary Diagnosis and Chief Complaint: A concise summary of why the patient is here.
- Past Medical History: Significant co-morbidities that impact current care.
- Current Assessment Findings: Head-to-toe assessment, including any changes from baseline.
- Vital Signs and Trends: Recent vital signs, pain assessment, and any significant patterns.
- Medications and IV Fluids: Current list, recent administration, and any pending doses.
- Laboratory and Imaging Results: Critical results, pending tests, and their implications.
- Treatment Plan and Interventions: Physician orders, consults, and nursing care plan.
- Pending Tasks and “To-Dos”: What still needs to be done on the upcoming shift.
- Code Status and Family Dynamics: Advance directives, family involvement, and social issues.
- Anticipated Discharge Plan: What steps are being taken for discharge readiness.
Tips for Implementing Your New Nurse Hand Off Report Template Effectively
Rolling out a new system, even one as beneficial as a standardized nurse hand off report template, requires thoughtful planning and execution. The key to successful implementation lies in fostering acceptance and demonstrating the practical advantages to the nursing staff. Start by involving nurses in the template’s design or customization process. Gathering their input ensures the template is user-friendly and addresses their specific needs and workflow, making them feel invested in its success rather than feeling like another top-down directive.
Once the template is finalized, comprehensive training is essential. Don’t assume everyone will intuitively understand how to use it. Provide clear, concise education on each section of the template, explaining its purpose and how to accurately complete it. Consider offering hands-on practice sessions and pairing less experienced nurses with seasoned mentors to guide them through the initial uses. Emphasize how the template streamlines their work and improves patient outcomes, rather than simply being another task to complete.
Finally, remember that implementation is an ongoing process, not a one-time event. Regularly solicit feedback from nurses using the template. Are there areas that are confusing? Is anything missing? Is it too cumbersome? Be prepared to make small adjustments based on their experiences. Continuous evaluation and refinement will ensure the template remains a valuable, dynamic tool that truly supports efficient, high-quality patient care and becomes an indispensable part of your unit’s routine.
Embracing a structured approach to shift changes fundamentally elevates the standard of patient care. By providing a clear, comprehensive pathway for information exchange, healthcare teams can ensure that every patient receives continuous, well-informed attention. This commitment to thorough communication not only fosters a safer environment for patients but also empowers nurses with the confidence and tools they need to excel in their vital roles, ultimately strengthening the entire care continuum.