In the dynamic and often complex environment of psychiatric care, effective communication stands as the bedrock of patient safety and continuity of treatment. Every shift brings new insights, observations, and interventions, and accurately relaying this information is paramount for the incoming team. Without a structured approach, crucial details can be overlooked, potentially impacting patient outcomes and staff efficiency.
Think about the fast pace of a busy unit and the sheer volume of information a nurse processes in a single shift. From medication adjustments and therapeutic interventions to subtle shifts in a patient’s mood or behavior, every piece of data is a puzzle piece in their recovery journey. Ensuring that these pieces are seamlessly transferred from one shift to the next is not just good practice; it is an ethical imperative.
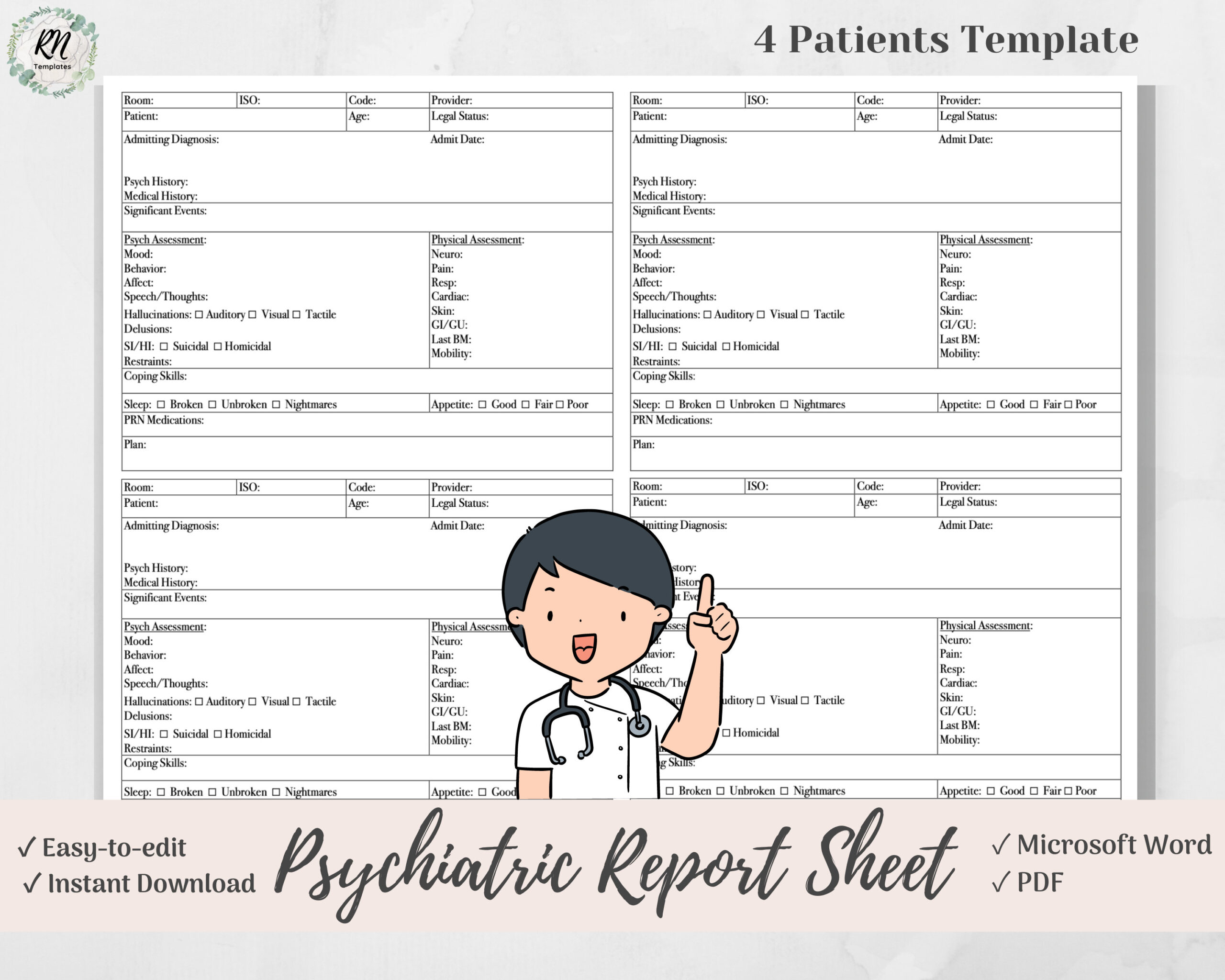
This is precisely where a robust psychiatric nursing shift report template becomes an invaluable tool. It’s more than just a form; it’s a critical component of interdisciplinary communication, helping to standardize the handover process and ensure that no vital information gets lost in translation. Let’s explore how a well-designed template can transform your shift reports and elevate the standard of care.
Crafting the Core: Essential Elements of a Powerful Shift Report
A comprehensive shift report in psychiatric nursing isn’t just about listing events; it’s about painting a holistic picture of the patient’s status, progress, and immediate needs for the next team. It needs to be clear, concise, and most importantly, relevant. The goal is to provide the incoming nurse with all the necessary information to pick up where the previous shift left off, ensuring seamless and safe care. Without a structured approach, the handoff can become fragmented, leading to missed details or an incomplete understanding of a patient’s evolving condition.
Consider the delicate nature of psychiatric care, where a patient’s mental status can fluctuate rapidly, and subtle cues can hold significant meaning. An effective psychiatric nursing shift report template guides the reporting nurse through all critical areas, prompting them to address every aspect that contributes to a patient’s well-being and risk profile. It moves beyond merely reporting what happened to explaining the “why” and “what next,” fostering a proactive approach to patient management.
The structure provided by a template acts as a safety net, reducing the chances of crucial information being forgotten during a hurried handover. It ensures that every patient, regardless of their presenting issues, receives the same diligent review during the reporting process. This consistency is vital for maintaining high standards of care across all shifts and for every member of the nursing team. It also serves as a valuable document for future reference, offering a clear snapshot of a patient’s journey through different shifts and interventions.
Critical Sections to Include in Your Template
- Patient Demographics and Admission Information: Briefly review the patient’s name, age, diagnosis, and date of admission. This sets the stage for the rest of the report.
- Current Mental Status Assessment: This is arguably the most important section in a psychiatric report. Detail appearance, mood, affect, thought process, content (e.g., delusions, hallucinations), perception, insight, judgment, and level of consciousness. Note any significant changes from previous assessments.
- Safety Concerns and Risk Assessment: Crucial for psychiatric units. Document any current or past suicidal ideation, homicidal ideation, self-harm behaviors, elopement risk, aggression, or other safety concerns. Include specific interventions implemented to mitigate these risks.
- Medications and PRN Effectiveness: List current medications, recent changes, and the effectiveness of any PRN (as-needed) medications administered, noting the reason for administration and the patient’s response.
- Therapeutic Interventions and Responses: Describe any one-on-one sessions, group therapy participation, behavioral interventions, or de-escalation techniques used, along with the patient’s response to these interventions.
- Treatment Plan Progress and Goals: Update on the patient’s progress towards their treatment goals, any observed barriers, and new goals established during the shift.
- Physical Health Status: Briefly cover any new physical complaints, vital sign abnormalities, pain management needs, or changes in sleep, appetite, or elimination patterns.
- Discharge Planning and Social Support: Note any updates on discharge planning, involvement of family or social supports, and community resource referrals.
- Any New Orders or Consults: Report any new physician orders, consults placed (e.g., social work, psychology), or diagnostic tests pending.
By systematically addressing each of these points, the template ensures a thorough and consistent review of the patient’s condition, promoting clear communication and collaborative care. This structured approach helps incoming nurses prioritize care, understand immediate risks, and continue the therapeutic process without interruption.
Streamlining Communication: Tips for Effective Template Utilization
Having a robust psychiatric nursing shift report template is only the first step; its true value comes from consistent and effective implementation. To truly optimize its use, nurses should embrace it not just as a checklist but as a tool for storytelling – a concise, factual narrative that empowers the next caregiver. Encourage a culture where the template is seen as a vital part of patient advocacy, fostering an environment of accountability and shared responsibility for patient outcomes.
One key aspect of effective utilization is training. All nursing staff, regardless of experience level, should be thoroughly trained on how to accurately and efficiently complete the template. This includes understanding the nuances of documenting mental status, risk assessments, and intervention responses. Regular audits and feedback sessions can help refine the process, identify areas for improvement, and ensure that the template is being used to its fullest potential, aligning with the unit’s specific needs and patient population.
Furthermore, integrating the template into your daily workflow, perhaps through an electronic health record system, can significantly enhance its utility. Digital templates can offer features like auto-population of demographic data, standardized dropdown menus for common observations, and real-time updates. This not only saves time but also reduces transcription errors and improves legibility, ensuring that the information conveyed during handoff is always precise and easily accessible.
The implementation of a standardized psychiatric nursing shift report template is a transformative step for any psychiatric unit. It moves beyond simply relaying information to creating a comprehensive, clear, and consistent narrative that supports patient safety and therapeutic progress. By embracing a structured approach, nursing teams can significantly enhance communication, reduce errors, and foster a more collaborative and effective care environment.
Ultimately, a well-utilized template empowers nurses to deliver higher quality, more informed care. It ensures that every patient’s unique journey is thoroughly documented and seamlessly transitioned between shifts, allowing the focus to remain firmly on recovery and well-being. This commitment to clear and structured reporting cultivates a safer and more responsive healthcare system for both patients and dedicated nursing professionals.



